Physical Therapists in These 10 States Need to See This

The Physical Therapy Licensure Compact introduced in 2014 has just met the requirements it needs to allow licensed PTs to provide care across these state boundaries. These are the ten states currently in the compact: – Oregon (The first state to join!) – Arizona – Kentucky – Mississippi – Missouri – Montana – North Dakota […]
Texas Senate Bill Tackles Huge Telemedicine Hurdle

After a six-year conflict between the Texas Medical Board and Teladoc, Texas lawmakers just removed a state rule requiring providers to have a face-to-face consultation before providing telemedicine services. This changes the game for residents in who and how those patients access healthcare. [BACKGROUND] In 2011, the Texas Medical Board sent a letter to Teledoc […]
The House Passed the AHCA with a 217-213 vote, now what?

The Affordable Care Act that brought health coverage to millions of uninsured Americans is now being threatened by the GOP’s plan to Repeal & Replace. Under this new plan, our current law requiring insurers to accept all applicants, (at the same rates regardless of pre-existing conditions) is in the talks of being rolled back while […]
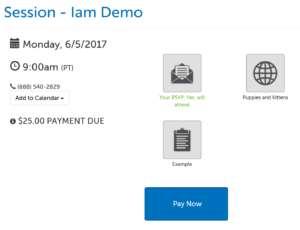
Release: require payment, session usage lookup, plan types
This article covers number of updates that we released this past weekend. Require Payment Users can now set a payment requirement when scheduling a session, so that participants cannot enter the session without first making the payment. To do so requires a little bit of setup: Connect a Stripe account. Set up an Account Service. […]